-
New research into treating inflammatory bowel disease shows the drug under the microscope is human poo. This novel treatment is called a faecal microbiota transplant (FMT) and it aims to manipulate gut bacteria through the transfer of healthy gut bacteria from donor to recipient. The idea is the transfer of faecal matter can help restore the balance of good bacteria in a recipient’s gut.
Previously, the treatment was limited to patients with severe bacterial infections, like Clostridium difficile, however, it is now being trialled on those with gastrointestinal disorders such as inflammatory bowel disease.
What’s inflammatory bowel disease?
Inflammatory bowel disease (IBD) refers to two conditions: Crohn’s disease and ulcerative colitis. Both affect the bowel, but in slightly different ways. Crohn’s disease can cause inflammation of the inner and outer lining of the bowel, and the digestive tract. Whereas ulcerative colitis inflames the inner lining of the bowel. Both are thought to be caused by a defect in the immune system, and while neither can currently be cured, both can be managed.
MORE: Can probiotics help with irritable bowel syndrome?
What’s gut bacteria?
The gut is made up of trillions of bacteria, known as the microbiota, which play a critical role in our overall health. In hand with producing vitamins, absorbing nutrients, and protecting against disease, the gut is home to most of our immune cells, an indicator of its fundamental role in our wellbeing.
As quoted in ABC's Lateline on 19 March 2014, the CSIRO's chief research scientist, Dr David Topping said "I think we're on the edge of something extraordinary. The attention has switched entirely to the large bowel bacterial population which we now know is absolutely critical to human health".
What role does gut bacteria play in inflammatory bowel disease?
Research over the last 10 years has shown people with inflammatory bowel disease have a distinctive gut microbiota composition. One recent study that examined the gut microbiota of 688 children who were newly diagnosed with Crohn’s disease found some potentially harmful microbial species were more abundant, and the number of beneficial microbial species were lower.
It’s still unclear whether these changes in the microbiota are the cause of IBD, or a result of the condition. However, it’s thought that faecal microbiota transplants may be able to change or improve gut microbiota, and reduce symptoms of IBD.
MORE: What to eat to keep your gut bacteria healthy
What is the research saying on faecal microbiota transplants?
Published research on FMT has doubled since 2012. To bring together these insights, researchers analysed 18 existing studies, which tested the treatment on 119 patients with IBD. The general aim of the studies was to manipulate the distinctive gut microbiota of IBD patients to prevent changes in the immune system, chronic inflammation (bleeding from the anus) and development of mucosal lesions (unusual skin growths).
Of the 119 patients, 54 achieved clinical remission, which meant symptoms did not present themselves again. However many of these studies were small and at risk of having skewed results. Based on these results, the researchers concluded that further research is needed to examine things like inflammatory bowel disease duration, environmental triggers, faecal donor selection, and preparation of faeces in regards to the effectiveness of FMT.
It’s fair to say there’s still a long way to go before we see faecal microbiota transplants used as a treatment for disease, however, there’s no doubt we’re on the brink of an exciting area of research that deserves further study. And perhaps with time, we’ll discover the true worth of our waste.
Visit Health Insights to read more about health research and trends.
Could human poo treat the incurable?

-
Innovating for members living with chronic disease
Medibank is supporting our members living with chronic diseases such as heart disease, arthritis, and diabetes, through our CareComplete programs.
-
Medibank’s palliative care at home trial
Giving our customers choice in where they would like to receive their end-of-life care can provide dignity, privacy and help them retain control over the care they receive.
-
How your phone habits affect your sleep
And what it means for your mental health, hormones and more.
-
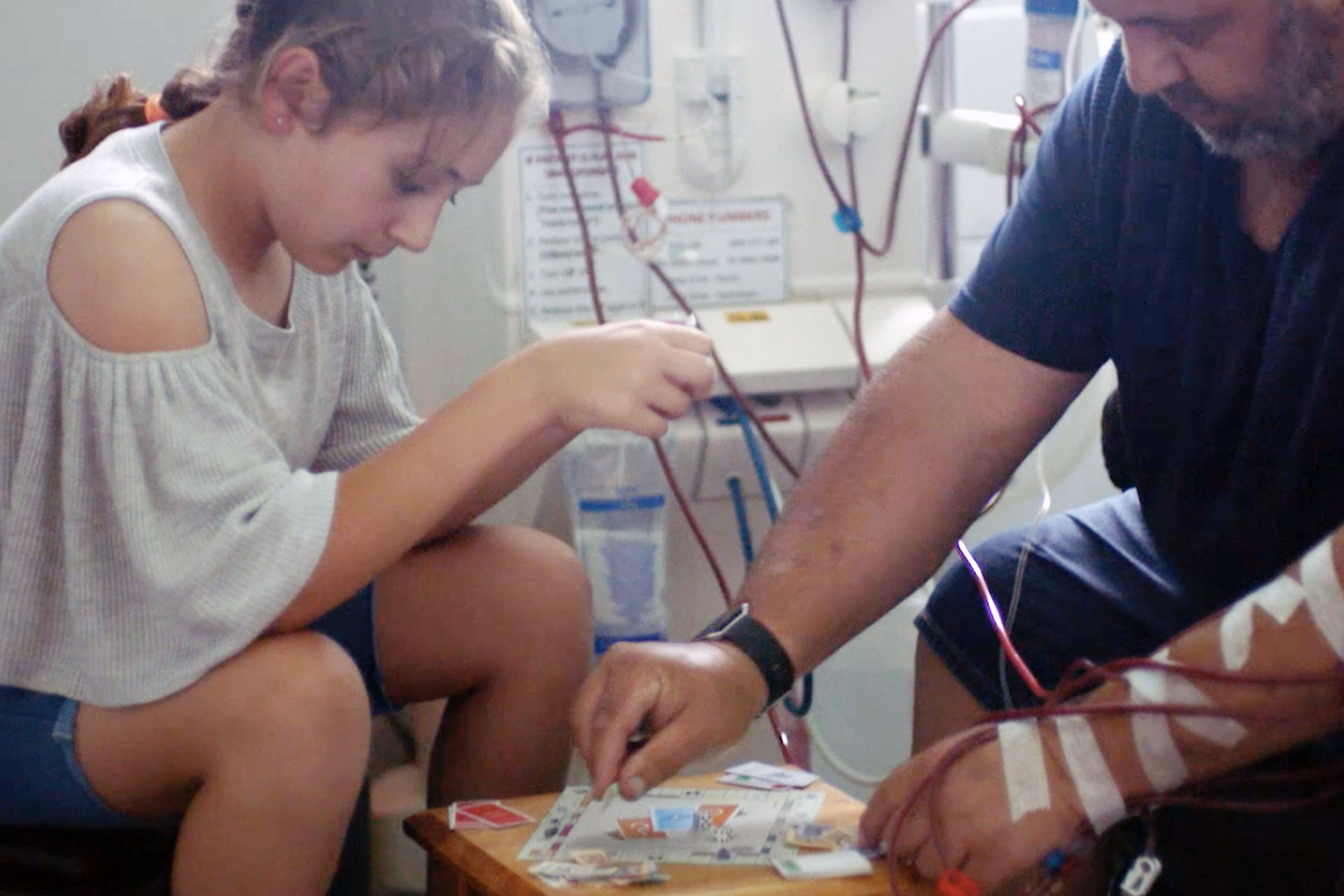
Medibank trialling haemodialysis at home
Giving members with chronic kidney disease more choice
-
The origins of western and eastern medicine
Two schools of thought explained
-
Almost half of hospital patients are looking for more support
Find out how Medibank is helping.
Subscribe to receive the best from Live Better every week. Healthy recipes, exercise tips and activities, offers and promotions – everything to help you eat, move and feel better.
By clicking sign up I understand and agree to Medibank's privacy policy